The drama is back downunder

A STEADY increase in the already-high rates of syphilis among gay men in Victoria is front and centre of the Victorian AIDS Council‘s (VAC) re-vamped Drama Downunder sexual health campaign.
Since its inception in 2008, the popular and eye-catching STI education series has continued to urge gay men and men who have sex with men (MSM) to undertake regular testing for a range of infections.
Now rolled out on a national scale every year, the campaign aims to focus attention on emerging sexual health problem areas within the community.
Its primary goals of raising awareness of STI transmission and de-stigmatising testing and treatment are aided by a combination of sex-positive imagery and messages, according to VAC health promotion director Colin Batrouney.
“The [Drama Downunder] campaign has been the most successful sexual health and testing campaign that VAC has implemented,” he said.
“People have found the campaign’s blend of sexual health awareness and humour both refreshing and provocative.
“Every year we seek to re-conceptualise how the campaign is going to approach the issue of sexual health and this year we have embarked on quite a major refresh of the imagery.”
A gradual increase in the rates of syphilis in Victoria over the past few years have given the campaign creators cause for concern.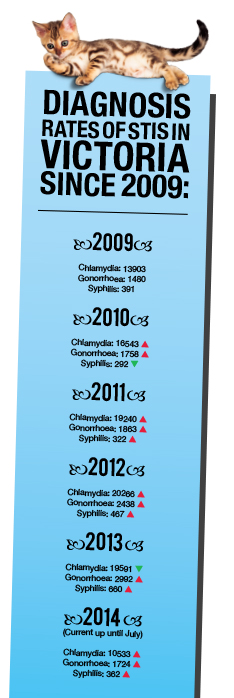
“Fourteen years ago there was virtually no syphilis,” said Chris Fairley, a public health professor at Monash University and Melbourne Sexual Health Centre director.
Batrouney added: “From 2010 through to the end of 2013, there was a 126 per cent increase in infectious syphilis notifications.”
According to Victorian Department of Health information, half-yearly rates for 2014 of 362 cases are already up over half of 2013’s total of 660 infections. In 2013, 76 per cent of syphilis transmission was via male-to-male sexual contact.
Symptoms for syphilis are not as obvious as other common STIs and often do not present themselves for weeks and months. Left untreated for years, the infection can cause severe damage to internal organs – and can even be fatal – but in the meantime, rashes and flu-like symptoms can emerge.
Fairley said the reasons behind the increase were unclear but the difficult nature and behaviour of the infection could be a contributing factor.
“Syphilis can be acquired through non anal sex – and often is – so while condoms substantially reduce the risk of acquiring it from anal sex, condoms are not used for oral sex which can also transmit it,” he said.
“It may be that clients are not recognising the symptoms as clearly as they could – and delaying presentation or possibly – not seeking treatment at all.
“The ulcers and rash usually resolve spontaneously without treatment – but people remain infectious during sex.”
According to Batrouney, the need for a wide-reaching campaign to be redeveloped and re-introduced each year is a necessity to keep the message of STI testing and treatment from becoming stale.
“It’s very important that we have a dynamic campaign around sexual health, and ideally, more than just one,” he said.
“It’s important for people to understand that if they want to continue to have great sex, then they need to maintain their sexual health, not just for themselves, but also for the health and wellbeing of their sexual partners, even if that is just one other person, or a hundred.”
Fairly said relevant and current education campaigns are some of the key necessary components to tackling rates of STIs in the community.
“One of the most important factors that determine how common a sexually transmitted infection is in a community is how accessible health care is,” he said.
“Accessible health care has two aspects. First, that health care is there to access – which is why free STI clinics are important – but a second really important issue is that the community knows what symptoms suggest they have caught an STI, so they can access treatment as soon as possible after symptoms begin.
“Also, understanding when they need to have screening tests is also important.”
The campaign creators also believe keeping rates of STIs under control and raising awareness of treatment are also relevant in tackling HIV and AIDS, as managing the two are seen to work hand-in-hand.
“A simple blood test can test for HIV and syphilis – so if someone wants (a blood test) only then that is fine… every three-to-six months is ideal. Swabs are recommended, also,” Fairley said.
However, increasing rates of STIs are not solely a Victorian problem, and Batrouney said that when VAC’s new campaign becomes national again, it would add to the strength of the message.
“All jurisdictions are facing similar challenges with regard to increased rates of syphilis and other STIs,” he said.
“If Drama Downunder continues to be run nationally, its strength is really in the consistency of messaging: ‘Sexy Health is Easy, Get Tested, Get Treated, No Drama!’”
For more information, visit www.thedramadownunder.info