‘Limit Sexual Partners’ To Reduce Mpox Transmission, Says Chief Health Officer

Mpox numbers continue to rise across Australia, with 152 cases recorded this year so far – and Chief Health Officer of Victoria, Dr Clare Looker, has advised keeping records of sexual partners for contact tracing, and limiting sexual contact.
Victoria has the largest outbreak with 83 cases – 21 of which were reported in the last fortnight.
NSW, Queensland and Victoria have issued health alerts in response to the rise in infections.
Rhonda Stuart, director of public health and infection prevention at Monash Health in Victoria told the ABC the virus re-emergence was likely due to the public dropping their guard, rather than a new virus strain.
“There’s a fear when something new comes so it initially creates behavioural change, but like with COVID we got vaccines and then got on with our normal lives,” she said.
Cases surpass the 2022 outbreak
Australia’s first Mpox outbreak in 2022 led to 144 cases, mainly from international travellers. Vaccinations and public health measures contained the outbreak, leading to only 26 cases being reported in 2023.
This year, local transmission is the primary cause of infections rather than international travel. New South Wales issued a safety notice last week with 22 cases reported over three weeks. Queensland raised an alert in May with 10 locally acquired cases, now at 17. Victoria’s outbreak has reached 83 infections, with about 90% locally acquired.
Getting mpox vaccination is only the start
On SBS radio, Professor Stuart urged the public against complacency. “This is really important for people to understand. The Mpox vaccine certainly decreases the risk of getting Mpox, and really decreases the risk of severe symptoms, but we do know that people who are double vaccinated are still getting Mpox if they’re still in that risk group and getting lots of contacts.”
“So don’t assume that your double vaccination doesn’t mean you can’t get Mpox, and you still need to seek treatment or seek a test to see what’s going on.”
Peter Locke, the director of HIV and clinical support services at Thorne Harbour, told the ABC “We now have plenty of vaccine available across Australia, and eligibility for vaccination has recently been expanded … The vaccine is free, and you don’t need Medicare.”
Thorne Harbour has set up free vaccination clinics across Melbourne, with hundreds of people attending in recent weeks. Vaccinations are given in two doses, 28 days apart, reducing the risk and severity of mpox.
Advice: limit sexual partners & contact tracing
Dr Looker advised that individuals at risk of infection could consider further ways of limiting transmission during the current wave.
“The recent rise in cases means we also want people to think about reducing their risk in other ways, which could mean limiting the number of intimate partners, and ensuring they’re sharing contact details to help with contact tracing if needed,” Looker explains.
Professor Stuart stated “We are hopeful it can be contained – it was contained in 2022 … but we do need help from the public to do that. Vaccination, getting tested soon, making sure partners are all notified and aware that they could present with symptoms are really really important.”
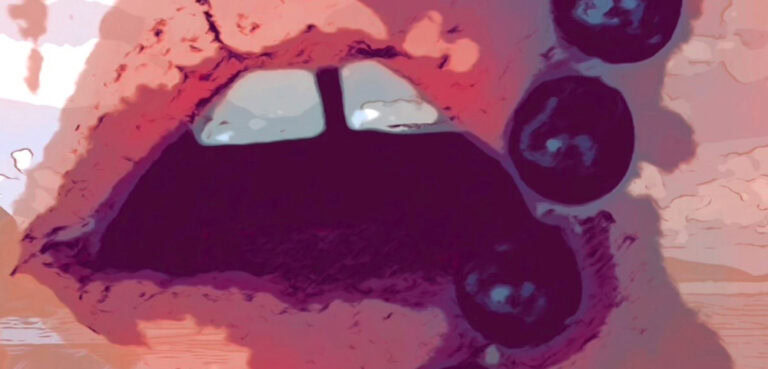
Mpox: What to look out for
Thorne Harbour Health notes that current outbreak symptoms can be less obvious, and can be mistaken for other sexually transmitted infections.
Professor Stuart says that the rash usually appears where contact has occurred. “Mpox is a viral infection that causes a nasty rash, and it can also cause systemic symptoms such as fever and aches and pains, but the rash is the thing that is most common with Mpox. Depending on where the rash is it can cause intense pain.”
Mpox is not a part of usual STI screenings, and must be requested especially from doctors.